Pancreatic Cancer
Pancreatic cancer (cancer of the pancreas) mainly occurs in people aged over 60. If it is diagnosed at an early stage then an operation to remove the cancer gives some chance of a cure. In general, the more the cancer has grown and spread (the more advanced the cancer), the less chance that treatment will be curative. However, treatment can often slow the progress of the cancer.
Understanding the pancreas
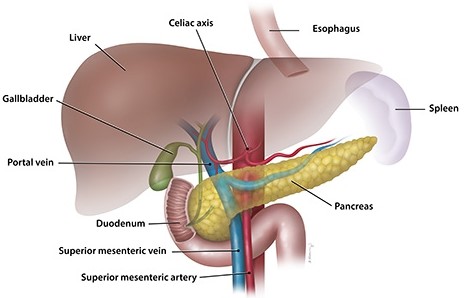
The pancreas makes a fluid that contains chemicals (enzymes) that are needed to digest food. The enzymes are made in the pancreatic cells and are passed into tiny tubes (ducts). These ducts join together like branches of a tree to form the main pancreatic duct. This drains the enzyme-rich fluid into the duodenum. The enzymes are in an inactive form in the pancreas (otherwise they would digest the pancreas). They are activated in the duodenum to digest food.
Groups of special cells called islets of Langerhans are scattered throughout the pancreas. These cells make the hormones insulin and glucagon. The hormones are passed (secreted) directly into the bloodstream to control the blood sugar level.
The bile duct carries bile from the liver and gallbladder. This joins the pancreatic duct just before it opens into the duodenum. Bile also passes into the duodenum and helps to digest food.
An insight into cancer
Cancer is a disease of the cells in the body. The body is made up from millions of tiny cells. There are many different types of cell in the body and there are many different types of cancer, which arise from different types of cell. What all types of cancer have in common is that the cancer cells are abnormal and multiply out of control.
A malignant tumour is a lump or growth of tissue made up from cancer cells, which continue to multiply. Malignant tumours invade nearby tissues, which can cause damage. Malignant tumours may also spread to other parts of the body. This happens if some cells break off from the first (primary) tumour and are carried in the bloodstream or lymph channels to other parts of the body. These small groups of cells may then multiply to form secondary tumours (metastases) in one or more parts of the body. These secondary tumours may then grow, invade and damage nearby tissues, and spread again.
Some cancers are more serious than others, some are more easily treated than others (particularly if diagnosed at an early stage), some have a better outlook (prognosis) than others. So, cancer is not just one condition. In each case it is important to know exactly what type of cancer has developed, how large it has become and whether it has spread. This will enable you to obtain reliable information on treatment options and outlook.
Pancreatic cancer at a glance
Pancreatic cancer is relatively uncommon. It develops in about 1 in 10,000 people each year. There are several types of pancreatic cancer but more than 9 in 10 cases are ductal adenocarcinomas.
Ductal adenocarcinoma of the pancreas
This type of cancer develops from a cell which becomes cancerous in the pancreatic duct. This multiplies and a tumour then develops in and around the duct. As the tumour enlarges:
It can block the bile duct or the main pancreatic duct. This stops the drainage of bile and/or pancreatic fluid into the first part of the gut, known as the duodenum.
It invades deeper into the pancreas. In time it may pass through the wall of the pancreas and invade nearby organs such as the duodenum, stomach or liver.
Some cells may break off into the lymph channels or bloodstream. The cancer may then spread to nearby lymph nodes or spread to other areas of the body (metastasise).
Other types of pancreatic cancer
There are some rare types of cancer which arise from other types of cells within the pancreas. For example, cells in the pancreas that make insulin or glucagon can become cancerous (insulinomas and glucagonomas). These behave differently to ductal adenocarcinoma. For example, they may produce too much insulin or glucagon, which can cause various symptoms.
Causes of pancreatic cancer (adenocarcinoma of the pancreas)
A cancerous tumour starts from one abnormal cell. The exact reason why a cell becomes cancerous is unclear. It is thought that something damages or alters certain genes in the cell. This makes the cell abnormal and multiply out of control.
Many people develop cancer of the pancreas for no apparent reason. However, certain risk factors increase the chance that pancreatic cancer may develop. These include:
Ageing. It is more common in older people. Most cases are in people aged over 60.
Smoking.
Diet. Eating a diet high in fat and meat seems to increase the risk.
Obesity
Persistent inflammation of the pancreas (chronic pancreatitis)
Most cases of chronic pancreatitis are due to drinking a lot of alcohol. There are other less common causes.
Diabetes
Note: diabetes is common and the vast majority of people with diabetes do not develop pancreatic cancer.
Chemicals. Heavy exposure at work to certain pesticides, dyes and chemicals used in metal refining may increase the risk.
Genetic and hereditary factors
Most cases of pancreatic cancer do not run in families. However, some families have a higher incidence of pancreatic cancer than average. It is thought that about 1 in 10 pancreatic cancers are due to inheriting an abnormal gene. See your doctor if you are concerned that pancreatic cancer is common in your family. You may be offered screening tests with the aim of detecting pancreatic cancer at an early stage when the chance of a cure is high
The indications of pancreatic cancer
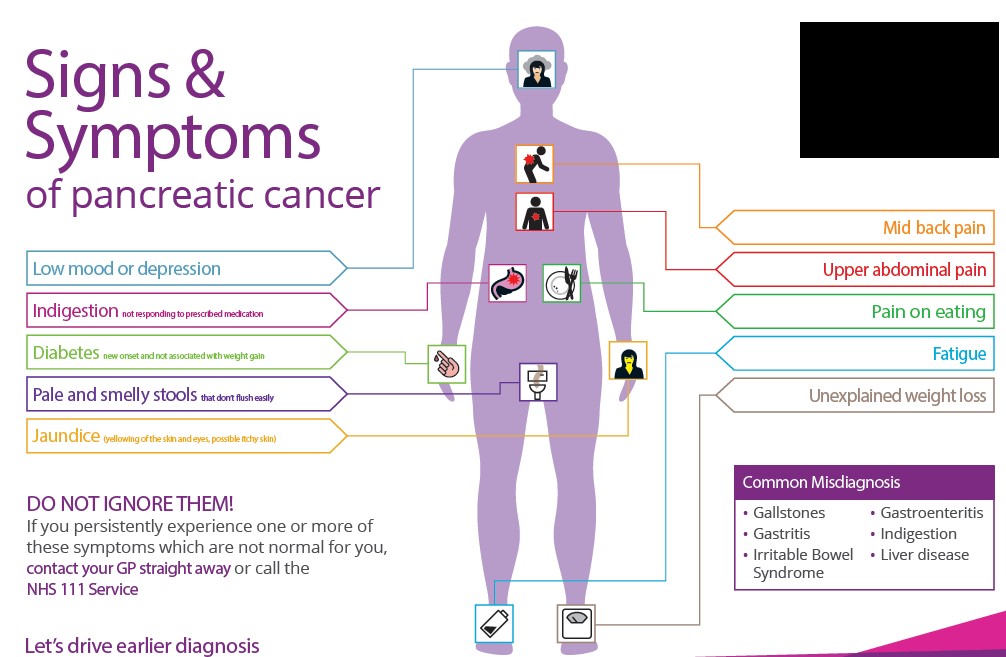
Symptoms of a blocked bile duct
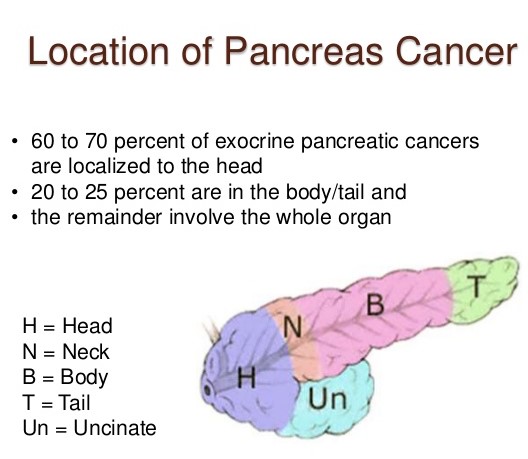
In about 7 in 10 cases the tumour first develops in the head of the pancreas. A small tumour often causes no symptoms at first. As the tumour grows it tends to block the bile duct. This stops the flow of bile into the first part of the gut, known as the duodenum, which leads to:
Yellow skin (jaundice) – caused by bile seeping into the bloodstream due to the blockage. Dark urine – caused by the jaundiced blood being filtered by the kidneys.
Pale stools (faeces) – as the faeces contain no bile which causes their normal brown colour. Generalised itch – caused by the bile in the bloodstream.
Pain is often not a feature at first. Therefore, a painless jaundice that becomes worse is often the first sign of pancreatic cancer. Feeling sick (nausea) and being sick (vomiting) are also fairly common symptoms.
Other symptoms
As the cancer grows in the pancreas, further symptoms that may develop include:
Pain in the upper tummy (abdomen). Pain can also pass through to the back.
You may feel generally unwell and lose weight. These symptoms are often the first to develop if the cancer develops in the body or tail of the pancreas (when the bile duct is not blocked).
You may not digest food very well, as the amount of pancreatic fluid will be reduced. This can cause smelly pale faeces and weight loss.
Rarely, diabetes develops if nearly all the pancreas is damaged by the tumour.
Rarely, a tumour can trigger inflammation of the pancreas (acute pancreatitis). This can cause severe abdominal pain.
If the cancer spreads to other parts of the body, various other symptoms can develop.
Diagnosis and assessment of pancreatic cancer
Initial assessment
There are many causes of yellow skin (jaundice) and of the other symptoms listed above – for example, a blocked gallstone or liver inflammation (hepatitis). Therefore, some initial tests are usually arranged if you develop jaundice or the other symptoms listed above. Typically, these include an ultrasound scan of the tummy (abdomen) and various blood tests. These initial tests can usually give a good idea if the cause of jaundice is a blockage from the head of the pancreas.
Assessing the extent and spread
If you are confirmed to have pancreatic cancer, or it is strongly suspected from the initial tests, further tests may be done to assess if it has spread. For example:
A computerised tomography (CT) scan is a commonly used test to assess pancreatic cancer. It is a specialised X-ray test that can give quite clear pictures of the inside of your body.
A magnetic resonance imaging (MRI) scan is sometimes done. An MRI scan uses a strong magneticfield and radio waves to create computer pictures of tissues, organs and other structures inside your body.
An endoscopic ultrasound scan (EUS) An endoscope (gastroscope) is a thin, flexible, telescope. It ispassed through the mouth, into the gullet (oesophagus) and stomach and on into the first part of the gut, known as the duodenum. The endoscope contains fibre-optic channels which allow light to shine down so the doctor or nurse can see inside. Some endoscopes are fitted with a tiny ultrasound scanner at their tip, which can obtain pictures of structures behind the gut, such as the pancreas.
A chest X-ray .
A laparoscopy.-This is a procedure to look inside your abdomen by using a laparoscope. Alaparoscope is like a thin telescope with a light source. It is used to light up and magnify the structures inside the abdomen. A laparoscope is passed into the abdomen through a small cut (incision) in the skin.
This assessment is called staging of the cancer. The aim of staging is to find out:
How much the tumour in the pancreas has grown and whether it has grown partially or fully through the wall of the pancreas.
Whether the cancer has spread to local lymph nodes.
Whether the cancer has spread to other areas of the body (metastasised).
By finding out the stage of the cancer, it helps doctors to advise on the best treatment options. It also gives a reasonable indication of outlook(prognosis)
Biopsy
A biopsy is a procedure in which a small sample of tissue is removed from a part of the body. The sample is then examined under the microscope to look for abnormal cells. If a biopsy is thought to be needed then one way to obtain a sample from the pancreas is to take the biopsy sample when you have an endoscopy. This is done by passing a thin grabbing instrument down a side channel of the endoscope (gastroscope). Alternatively, sometimes a biopsy is done at the same time as having a scan. It can take two weeks for the result of a biopsy.
What are the treatment options for pancreatic cancer?
Treatment options that may be considered include surgery, chemotherapy and radiotherapy. The treatment advised for each case depends on various factors, such as how large the cancer is and whether it has spread (the stage of the cancer) and your general health.
You should have a full discussion with a specialist who knows your case. He or she will be able to give the pros and cons, likely success rate, possible side-effects and other details about the various possible treatment options for your type of cancer.
You should also discuss with your specialist the aims of treatment. For example:
Treatment may aim to cure the cancer. Some pancreatic cancers can be cured if they are treated in the early stages of the disease. (Doctors tend to use the word remission rather than the word cured. Remission means there is no evidence of cancer following treatment. If you are in remission, you may be cured. However, in some cases a cancer returns months or years later. This is why doctors are sometimes reluctant to use the word cured.)
Treatment may aim to control the cancer. If a cure is not realistic, with treatment it is often possible to limit the growth or spread of the cancer so that it progresses less rapidly. This may keep you free of symptoms for some time.
Treatment may aim to ease symptoms. If a cure is not possible, treatments may be used to reduce the size of a cancer, which may ease symptoms such as pain. If a cancer is advanced then you may require treatments such as nutritional supplements, painkillers, or other techniques to help keep you free of pain or other symptoms.
Surgery
If the cancer is at an early stage then there is a modest chance that surgery can be curative. (An early stage means a small tumour which is confined within the pancreas and has not spread to the lymph nodes or other areas of the body).
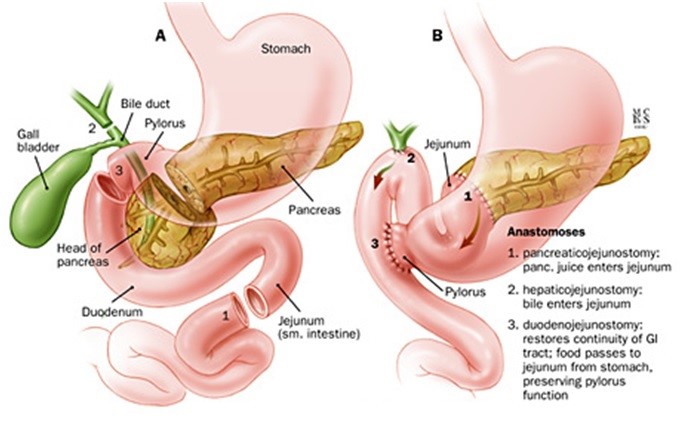
If the tumour is in the head of the pancreas then an operation to remove the head of the pancreas may be an option. This is a long and involved operation, as the surrounding structures, such as the first part of the gut, known as the duodenum, the stomach, the bile duct, etc, need to be rearranged once the head of the pancreas is removed.
If the tumour is in the body or tail of the pancreas then removal of the affected section of the pancreas is sometimes an option.
The reason why the chance of cure is only modest is because in a number of cases thought to be in an early stage, some cells have already spread to other parts of the body but are not yet detectable by scans or other staging tests. In time they grow into secondary tumours.
Chemotherapy
Chemotherapy is a treatment of cancer by using anti-cancer medicines which kill cancer cells or stop them from multiplying.. When chemotherapy is used in addition to surgery it is known as adjuvant chemotherapy. For example, following surgery you may be given a course of chemotherapy. This aims to kill any cancer cells which may have spread away from the primary tumour.
Radiotherapy
Radiotherapy is a treatment which uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells, or stops cancer cells from multiplying. Radiotherapy is not commonly used to treat pancreatic cancer.
The outlook (prognosis)
If a pancreatic cancer is diagnosed and treated at an early stage then there is a modest chance of a cure with surgery. As a rule, the smaller the tumour, and the earlier the tumour is diagnosed, the better the outlook. Some tumours which develop in the head of the pancreas are diagnosed very early, as they block the bile duct and cause yellow skin (jaundice) fairly early on. This obvious symptom is then investigated and surgery to remove a small tumour may be curative
However, most pancreatic cancers are advanced before they cause symptoms and are diagnosed. A cure is unlikely in most cases. However, treatment may slow down the progression of the cancer.